Medically reviewed by Sophia Yen, MD, MPH – Written by Pandia Health Editorial Team
Dr. Sophia Yen, CEO & co-founder of Pandia Health, often talks about how to stop your period when on the birth control pill. But do you know how to put this into practice? Read on to learn more about how to safely skip your period using birth control.

Is it safe to skip your period?
Contrary to popular belief, it is safe and practical for people with uteri to stop their periods when taking birth control. It is often believed that the uterine lining thickens and needs to be shed, so not having a period will lead to a dangerous build up. However, this is not the case when the individual takes hormonal birth control.
The bleeding that occurs when an individual takes birth control (usually during the days in which they take the placebo pill) is actually a withdrawal bleed, which is different from a period. This bleed is caused by the drop in hormones, rather than the shedding of the uterine lining. Furthermore, it is not medically necessary to experience this while taking birth control.
Why do most pill packs have a row of placebo pills?
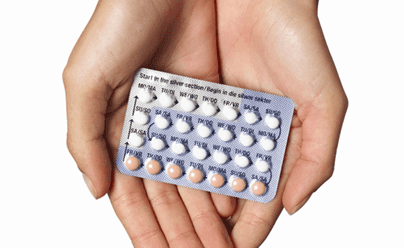
One of the inventors of the birth control pill, Dr. John Rock wanted women to have a period every month. It wasn’t until two of the co-founders questioned why this was necessary that skipping periods was even considered. However, Dr. Rock was insistent that those with uteri bleed every month because he believed that the Catholic Church would be more accepting if he kept it at status quo. He won the argument, and as a result, the placebo row is now included in most pill packs.
Thankfully, birth control pill users can simply skip the row of placebo pills and start their next pack as soon as they complete their current pack.
What are the benefits of skipping your period?
Skipping your period not only helps improve general well-being, but also long-term reproductive health. Not to mention the fact that period products are costly and often harmful to the environment!
In terms of well-being, skipping your period decreases symptoms associated with bleeding – cramps, bloating, headaches, anemia, acne, embarrassment… and that is just to name a few. Additionally, choosing not to bleed every month could lead to a lower risk of developing endometrial and ovarian cancers by changing the susceptibility of cells to infection. Lastly, by not having to purchase period products as often, you save money and contribute less to pollution (most pads and tampons end up in landfills).
While skipping your period is safe, you should talk to a doctor before starting the process to ensure that it’s the right decision for you. For instance, it is recommended that individuals who have been menstruating for less than two years keep getting a period, as they are likely still growing and estrogen could impact their height.
How to skip your period
To safely skip your period you can use:
- 1. The birth control pill.
- 2. The ring like NuvaRing
- 3. The birth control patch like Twirla or Xulane (can only use for 12 weeks in a row max)
- 4. The hormonal IUDs (30% chance of no periods).
- 5. Implant birth control like Nexplanon
- 6. The shot has a 75% chance of no periods after 3 shots.
How to skip your period taking the pill
Skipping your period when taking the pill is super simple. After you finish the three rows of active pills, skip the row of placebo pills and move on to your next pack. Typically, the last row contains sugar or iron pills, which are a different color than the hormone pills.
The first time you try this, you may experience breakthrough bleeding after a few months. This is usually harmless and does not mean that your birth control is no longer effective. If breakthrough bleeding occurs, stop taking the hormone pills for five days. During this time, you’ll have a withdrawal bleed as a result of the change in hormones – this will reset your uterus. On day six, regardless of whether you’re still bleeding, restart the hormone pills.
After your first breakthrough bleed occurs, you will likely go a longer stretch without having it again. As long as you keep taking active pills, you can eventually turn off your period. That being said, every person with a uterus is different and thus, might have a different experience.
Making #PeriodsOptional with other types of birth control
It is possible to skip your period with birth control methods other than the pill including the patch and the ring. Those who have an IUD or implant may also notice lighter periods, if any.
The Ring
NuvaRing is a small, flexible ring that gets placed inside the vaginal canal to release hormones that prevent pregnancy. It is worn for three to five weeks at a time and is typically followed by a seven-day break when a withdrawal bleed occurs. In order to avoid this bleed, simply skip the break and put in your new ring immediately after you finish your last one.
The Patch
The patch is a sticky tab containing hormones that is placed somewhere on the skin (i.e. your arm, back, stomach, or butt). It is worn for seven days and then replaced for two additional weeks. The fourth week usually entails a period, in which case the patch is not placed on the skin. If you do not want to bleed, skip the break and put on your new patch each week. It is important to note, however, that you should not skip your period for more than 12 weeks in a row while on the patch, as this can increase your risk of developing blood clots.
The Hormonal IUD
With the hormonal IUD, a small, flexible device that is inserted into the uterus, many individuals notice lighter periods. However, this is unpredictable because each person with a uterus responds differently. On the “regular strength” IUDs (Mirena/Liletta) 20-50% of individuals stop bleeding altogether.
The Implant
A similar percentage of individuals who use the implant, a thin rod that is placed inside the arm, stop bleeding monthly. However, it is more common for individuals to bleed irregularly and eventually experience lighter periods.
What’s the takeaway?
Skipping your period is now easier than ever with the help of hormonal birth control. With that said, it is still necessary to communicate with your healthcare provider so they can prescribe you the correct amount of medication. Thankfully, under the Affordable Care Act, most insurance plans should cover the extras.
How can Pandia Health help?
Speaking of skipping your period, Pandia Health promotes making #PeriodsOptional by educating people with uteri on the benefits of not bleeding every month. We further promote this message by providing a FREE delivery service to all 50 states. You can transfer a current prescription to our pharmacy and have it shipped right to your mailbox. We know you have #BetterThingsToDo than making an extra trip to the pharmacy.
Watch our CEO/Co-Founder Dr. Sophia Yen’s TED’s talk on making #PeriodsOptional, the science and safety of #FewerPeriods #NoPeriods
Disclaimer: This article, even if and to the extent that features the advice of physicians and medical practitioners, it is not, nor is it intended to be, a substitute for professional medical advice, diagnosis or treatment, and should never be relied upon for specific medical advice. Always seek the advice of your doctor/primary care provider for specific health needs.