Medically reviewed by Sophia Yen, MD, MPH – Written by Pandia Health Editorial Team
What Is an IntrauterineDevice (IUD)?
Before you get an IUD inserted, it is important to know what an IUD is and how it works. It’s always a good idea to understand as much as you can about what healthcare you are receiving so be sure to ask your doctor or provider any questions that you might have. This will also develop your health literacy – remember, knowledge is power!
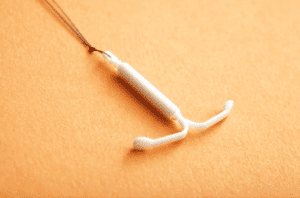
IUD stands for intrauterine device, which just means that it is a device that goes inside your uterus, the organ where a baby would develop. The IUD is T-shaped, flexible, and usually made of plastic. It is very small — only about the size of a quarter — which means you won’t even notice it’s there.
The IUD was first developed in the early 1900s, and became approved by the Food and Drug Administration (FDA) in the 1970s. IUDs became more mainstream in the early 2000s, and they are extremely popular now. By 2014, 14% of women ages 15-44 in the United States had IUDs.
There are two different types of IUDs both of which are effective at preventing pregnancy: hormonal and copper. Hormonal IUDs (Mirena, Liletta, Kylena, Skyla) prevent an embryo from ever happening by releasing the hormone progestin, which stops sperm by thickening the mucus in the cervix (the opening to the uterus), keeping the uterus lining thin so it can’t support a pregnancy, and sometimes blocking ovulation (the egg from coming out of the ovary).
On the other hand, copper IUDs (Paraguard) prevent sperm from reaching the egg because sperm is slowed down by copper. Regardless of which one you choose, know that IUDs are the most effective methods aside from a vasectomy and the implant.
Choosing the IUD Over Other Options
You might be wondering why you would choose an IUD instead of another birth control method such as the pill, patch, ring, implant or shot. The number of options might be overwhelming, but know that hundreds of those with uteri and their doctors have been through this process before. Plus, everyone’s body and priorities are different, so your experience may vary from another person’s but the aspects listed below are simple what those with uteri and their doctors most commonly consider.
The most important thing to know about IUDs is that, out of all of the reversible birth control methods, IUDs are the second most effective after the implant. With a hormonal IUD, the chance of pregnancy is 0.2% which means that out of every 1000 women with an IUD, only 2 will get pregnant; the copper IUD has an 0.8% chance of pregnancy, meaning just 8 out of 1000 women using the method will get pregnant. Essentially, with an IUD, you can rest assured that you will be very well protected against pregnancy.
Another advantage that sets IUDs apart from options like the pill is that it is long-acting and low maintenance. Once it is inserted, it doesn’t require any regular maintenance — you don’t need to take a medication or switch out a device. In fact, you might not even need to think about it for years! IUDs can stay in your uterus for three to ten years.
IUDs, particularly hormonal IUDs, also have limited side effects, and the majority of women do not experience any negative reactions. In fact, IUDs can have positive side effects – if you’re lucky, you can use an IUD to make your #PeriodsOptional. One in five women will not have any periods after getting an IUD and the remaining women are likely to experience lighter periods. Once your IUD is removed, your periods will return to as they were before; if you use the copper IUD, your periods will not stop, as no hormones are involved.
One downside of IUDs is that they require a medical procedure, which requires more of a time and physical investment than other birth control methods. However, this investment might be worth it for you because you won’t have to think about it for years. Like the pill, patch, ring, implant, and shot, the IUD does not protect against sexually transmitted infections (STIs). That means that if you have sex with a new partner (or even a longtime S.O.), you should use a barrier method such as a condom.
Types of IUDs
Out of the 2 options, the hormonal IUD is generally recommended, because it is more effective and tends to have fewer side effects. With the copper IUD, know that you might experience more bleeding and cramps during your periods.
In contrast, the hormonal IUD can make your periods go away or at least lighter. 30% of women on the hormonal regular dose IUD lose their monthly bleed, and the other 70% get lighter bleeds.
The copper IUD might be right for you if you don’t react well to hormones, because the copper IUD does not contain any hormones.
Either IUD can also work as emergency contraception (EC) up to 5 days after unprotected sex, making them the most effective EC and the best for females with a higher BMI.
Overall, it is best to discuss your medical history with your doctor to determine which option is the best for you.
How to Get an IUD
Now that you understand what an IUD is, how it works, and which one is right for you, it’s time to figure out how to get an appointment to have one inserted. A great place to go for an IUD insertion is your local Planned Parenthood, which provides high quality reproductive health care to people of all backgrounds. If you have a gynecologist, you can also ask them for an appointment; your primary care doctor can often put in an IUD (if they are family medicine, internal medicine, or adolescent medicine) or they can refer you to a gynecologist.
Most of the time, you won’t have to pay for the IUD or the cost of the appointment. Under the Affordable Care Act, insurance plans must cover IUDs. However, the insurance coverage by IUD brand can vary, so check with your health clinic to make sure you won’t have to worry about the cost. If you don’t have insurance, you can look into programs such as Medicaid or title X family Planning clinics. If you call your local Planned Parenthood clinic, they can also help you figure out how an IUD can be made affordable.
Preparing for the Appointment
Dr. Sophia Yen, our CEO and co-founder’s 3 Tips for decreasing pain during the IUD insertion:
- Scheduling your appointment during the last days of your period so that your cervix is already open.
- Ask for a paracervical block which will numb the area and should make insertion more comfortable.
- Pre-medicate with 600-800mg of ibuprofen WITH FOOD to minimize any pain.
After you’ve made your appointment to have an IUD inserted (congratulations!), it’s a good idea to take some time to understand what to expect during the procedure so that you can be prepared.
Before the insertion happens, the doctor will make sure that your body is ready by examining your vagina, cervix, and uterus. To be able to access your uterus, you doctor will use a speculum, which goes into your vagina. Then, she will insert the IUD into your uterus, leaving a string a few inches long that stays in your vagina. This process typically only lasts between five and fifteen minutes.
To prepare, you should drink water before your appointment so you do not get lightheaded during the procedure.It’s a good idea to come to the appointment with a friend, family member, or trusted adult so that they can drive you home and help you stay relaxed.
Staying Comfortable During the Appointment
Any medical procedure can be scary, especially if it’s one you haven’t experienced before. When you go into the exam room, remember that you have prepared for this -you’ve educated yourself about what you will experience, so now it’s time to relax. Your doctor has done this many times, and you are joining millions of women who also have IUDs. Take deep breaths, and if anything feels off, tell your doctor — she is there to make the procedure go as smoothly as possible.
After the appointment
You might feel some cramping after your IUD is inserted; this should not last long, and you can reduce the pain using a heating pad or ibuprofen. Your periods might also be irregular for the first few months, but, if you are on the hormonal IUD, they will become more regular and lighter with time. The IUD will provide protection against pregnancy as soon as it is inserted, so you can safely have sex at any time after the procedure.
You should keep in mind that some women have experienced their IUDs falling out, although this is very rare. If you think this has happened to you, call your doctor and they will help you determine if you need a new one. Otherwise, you won’t have to think about your IUD for the next few years.
Now, you can breathe a sigh of relief — you have taken an important step to protect yourself from pregnancy!
Disclaimer: The above information is for general informational purposes only and is NOT a substitute for professional medical advice. Always seek the advice of your doctor/primary care provider before starting or changing treatment.

