As Hannah Montana wisely stated, “everybody makes mistakes.” Or as we like to call it at Pandia Health, everybody has an ‘oopsies moment’. Usually, when Pandia Health is talking about an ‘oopsies moment’ we’re talking about unprotected sex.
So what is unprotected sex? Unprotected sex defined as the act of engaging in sexual intercourse without the use of condoms or any other forms of contraception (i.e IUD, implant, birth control pill). Whether it be the heat of the moment, or the choice to have unprotected sex –there are certain risks that unprotected sex brings, such as pregnancy and STD (sexually transmitted diseases).
Right After Having Unprotected Intercourse
Prevent Pregnancy
Anytime you have sex there is a risk of pregnancy, even if you got a surgical procedure (i.e tubal ligation, vasectomy being the chances 1/1000). This includes the age-old method that is affectionately referred to as the ‘pull out method,’ which refers to when the penis is removed from the vagina before ejaculation. While this method may seem foolproof, women can get pregnant from pre-ejaculate a.k.a. “pre-cum”, the semen that ‘leaks’ out before ejaculation. Pre-ejaculate can contain 10,000 sperm!
So how can you prevent pregnancy after an instance of unprotected sex? Your chances of getting pregnant vary throughout your 28 day menstrual cycle. You are most likely to get pregnant if you have unprotected sex during ovulation, which falls within your fertile window. Your fertile window occurs 5 days leading up to ovulation, the day of ovulation, and the day after ovulation –totalling a 7 day window. Having unprotected sex after or right before your period still runs you the risk of pregnancy, but the risk is slightly lower. However, not all is lost! After an instance of unprotected sex, you can take emergency contraception. With emergency contraception, you have a few options. Let’s review them from most effective to least effective:
Note that all methods can be use up to 5 days after unprotected sex or vaginal sexual assault. However, the emergency contraceptive pill methods are best used ASAP e.g. if the condom pops at 3am, we want the medicine in the uterine-bearing person at 3:10 am. No cuddling, snuggling, waiting until “the morning after.”
Copper IUD
The most effective emergency contraceptive is a copper IUD. It works equally well throughout if you get it inserted within 5 days of unprotected sex. This requires a visit to a doctor to have it inserted, and has no BMI limitation –making it the only real option for women with a BMI over 35. You can go to your primary care doctor, gynecologist, local Planned Parenthood or emergency room to get one inserted but call ahead to make sure they have it available and someone that can insert it. A benefit of choosing the copper IUD as an emergency contraceptive method is that you can keep it in for 10 to 12 years as a birth control method.
Hormonal IUD (52 mg)
Has no BMI limitation that we know of. Has a failure rate of 3/1000 people who use it. If choosing this birth control method for emergency contraceptive, you can keep the hormonal IUD in for 7 years for birth control purposes.
Ella
Pandia Health‘s expert birth control doctors’ pick for emergency contraception is Ella! While Ella is not over the counter, you can get a prescription from us here at Pandia Health or ask your doctor when you get your check up or birth control. We love Ella because it beats Plan B and its generics at every time point, meaning it is better at preventing pregnancy and it works for those with a higher BMI, up to 35. It also has a longer efficacy window, up to 5 days after unprotected sex. Also, because under the Affordable Care Act, if you have insurance, “it’s free” = no copay no deductible. One thing to note, if you are taking the birth control pill, patch, or ring, you should stop taking/using it and wait till 5 days after you’ve taken Ella. If you do not do this, you run a big risk of Ella not working, because the progestin in your pill, patch, ring blocks the Ella from working.
Order Emergency Contraception Online
Need emergency contraception? Order now and get peace of mind with discreet and reliable delivery. Don't wait, take control of your reproductive health today!
Plan B and its generics (levonorgestrel 1.5 mg)
You’ve probably heard about Plan B before, or as it’s lovingly called the ‘morning after pill.’ This option can be bought over the counter for about $50, or $24 if you choose a generic equivalent (e.g. New Day). While this is a great option if you are in a pinch, Plan B is not so effective for those with a BMI over 26, and completely ineffective for those with BMIs 30 or more. Additionally, while other emergency contraception can be taken up to 5 days after unprotected sex, Plan B works best when taken ASAP.
The Yuzpe Method (a whole bunch of birth control pills now and again in 12 hrs)
If you have a pack of birth control pills with levonorgestrel or norgestrel, you can take however many pills it takes to get to 100 mcg of ethinyl estradiol and 1mg of norgestrel or 500 mg of levonorgestrel ASAP and again in 12 hours. The negatives: this is the LEAST effective emergency contraception method, but it’s better than nothing. You could start with this and then go get an IUD for emergency contraception.
STD: Watch for Symptoms, Get Tested!
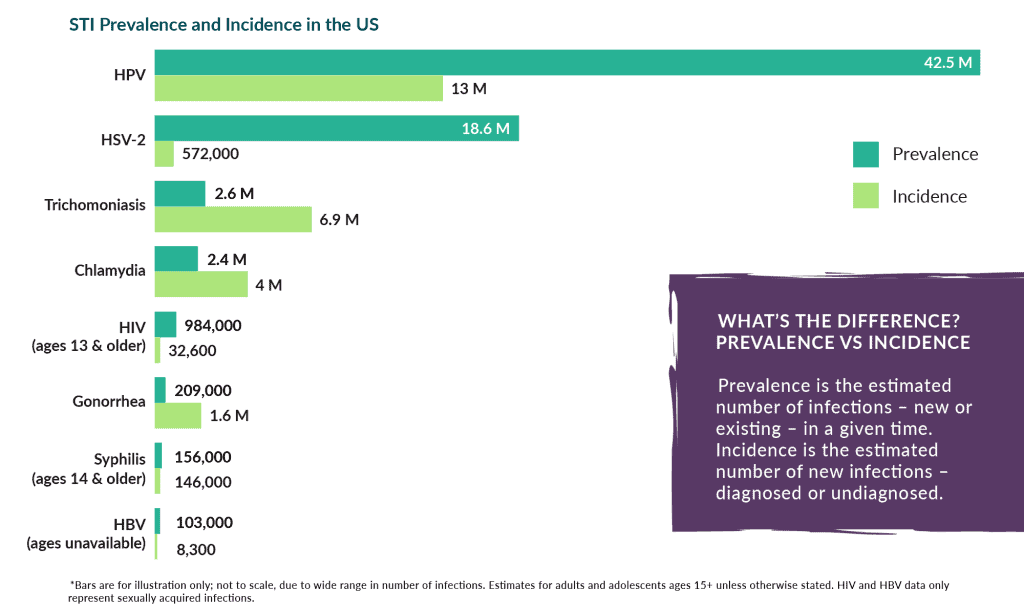
The second risk unprotected sex gets you is contracting an STI, or sexually transmitted infection. Some of the most common STIs are:
- HPV: Human Papilloma Virus it the most common STI. There is a vaccine for it that prevents 9 of the 150+ strains (not covering you from the other 141+ stains). HPV results in abnormal pap smears and potentially cervical cancer.
- Chlamydia: is a common, treatable STD that can cause infection among both men and women. Most people with Chlamydia have no symptoms. Symptoms of Chlamydia include:
-
-
- unusual
- /bleeding between discharge
- burning sensation while urinating
- vaginal soreness
-
- Gonorrhea: is a common, treatable STI that can cause infection in the genitals, rectum, and throat. 20-75% of people with gonorrhea do not have any symptoms. Symptoms of Gonorrhea include:
-
- new vaginal/penile discharge
-
- pain/burning while urinating
- rectal discharge, itching, soreness, or bleeding
- painful bowel movements
- Trichomoniasis is a very common, treatable STI caused by Trichomonas Vaginalis. Most people do not know that they have this condition, because only ~30% of infected individuals have symptoms. 2% of women and 0.5% of men have Trichomoniasis. Symptoms of Trichomoniasis include:
-
- unusual vaginal discharge with a fishy smell
- genital itching, burning, redness, or soreness
- discomfort while urinating
Ideally, before any sexual intercourse,you and your partner should discuss both of your sexual history and get tested for STIs. It is especially important because many STIs are silent and asymptomatic, so you or your partner could have an STI without knowing. Luckily, STI testing has been made easier with at-home test kits, like the one we offer. Our STI test kit screens for Chlamydia, Gonorrhea, and Trichomoniasis. If you’re nervous about discussing STIs with your partner, a fun date idea would be getting tested together and sharing your results!
Concerned about STI?
Buy now your Simple Health STI test kit and get safely tested at home.
- FREE delivery
- Prepaid envelope to send sample to a certified Laboratory
- Results within 24 hours
- Don't wait to get tested!
Is important to know that the STI tests are limited by what you are testing for. If you didn’t test for HIV, HSV, Syphilis, then you don’t know if you have them or not. To test for them you will need to see a provider in person. Most doctors don’t test for HSV (herpes), so make sure you ask for it if you go for in person testing to your doctor or provider. For those with penises there is NO commercial test for HPV (the MOST common STI).
Much like emergency contraception, if you have been recently exposed to HIV, you can take PEP within 72 hours to decrease the risk of the HIV infection.
Regardless, if you do get an STI –don’t panic! Most STIs can be managed with proper medication and precautions. However, in general there is NO cure for the viral STIs such as Herpes, HIV, HPV but you can take precautions to prevent infecting others and there are medications to decrease symptoms.
Get tested for pregnancy
Our Co-Founder, Dr. Sophia Yen says “act like you’re pregnant” until you get that period or negative pregnancy test, meaning if you would continue the pregnancy, do not drink alcohol, smoke cigarettes, vape, do illegal drugs. Do not test for pregnancy until the first day of your missed period. If you test before then, you might get a false negative, meaning it says you’re not pregnant but you are pregnant.
Still Concerned About Pregnancy or STD?
If you are still worried about potential pregnancy or STDs, your best option is to go see a doctor! While it may feel embarrassing at the time to talk to your doctor, there is absolutely no shame in it. Doctors exist to help you be your best self, and there is no room for judgment in the stirrups girl! Skip the stigma and stay on top of your reproductive health by seeing a medical professional when you are worried about potential pregnancy or STDs.
Be Safe, Stay Protected
Ok, so you’ve made it through the scariest part –you peed on cups and sticks and got your results back. Now, how can you avoid this happening in the future? You can double up on birth control methods by using condoms PLUS getting on hormonal birth control such as the pill, patch, ring, implant, or IUD or the non-hormonal copper IUD. Additionally, keep your STI status updated by regular screening. The USPSTF recommends those under 25 get checked at least once a year for gonorrhea and chlamydia.
Final Thoughts
Ok, so hopefully you’ve gotten everything you could from this article. There is no need to panic, simply take the next steps necessary to your situation and adjust accordingly. It is important that you know all of your reproductive health options ahead of time, so when an ‘oopsie’ occurs –you aren’t left scrambling. So, stock up on some emergency contraception and some at-home STI kits and be on your merry way!
Disclaimer: This article, even if and to the extent that features the advice of physicians and medical practitioners, it is not, nor is it intended to be, a substitute for professional medical advice, diagnosis or treatment, and should never be relied upon for specific medical advice. Always seek the advice of your doctor/primary care provider for specific health needs.