Written by Giuliana Castellucci, medically reviewed by Sophia Yen, MD, MPH.
TL;DR: How Birth Control Affects Menopause Symptoms
Hormonal birth control methods (like pills, patches, and rings) can mask menopause symptoms by stabilizing hormone levels, making it challenging to recognize the transition into menopause. While these methods may reduce symptoms such as hot flashes and mood swings, they can also obscure signs like irregular periods. To determine if you’ve reached menopause, consult your healthcare provider; they may recommend pausing birth control to assess your natural cycle. It’s generally advised to stop hormonal birth control by age 55, as the likelihood of pregnancy becomes minimal.
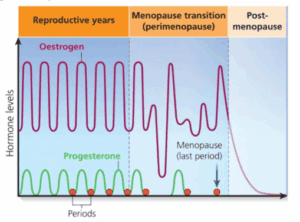
If you’re using hormonal birth control, like the pill, it can mask the typical signs of perimenopause and menopause. That’s because birth control pills provide a stable level of hormones, making it harder to recognize when your body is starting the transition into menopause.
Here’s what’s happening behind the scenes:
- The estrogen/progesterone birth control pill stabilizes estrogen and progestin levels, which prevents irregular periods and hot flashes (two of the major signs of perimenopause).
- Birth control pills, patches, and rings (containing estrogen and progesterone) prevent the hormonal fluctuations that typically trigger many perimenopause and menopause symptoms.
- Most women experience fewer or no mood swings, lighter/no periods, and fewer or no night sweats because of hormonal birth control like the pill/patch/ring—even while their body begins transitioning.
This means that while your body may be undergoing hormonal changes, birth control pill, patch, ring can smooth over or even completely hide/prevent symptoms.
Another way to put it, the “birth control” pill, patch, ring is hormonal treatment for perimenopause and is actually the preferred treatment in someone who also needs birth control or who prefers a smooth hormonal system vs the “chaos of perimenopause.”
How to Know If I’ve Reached Menopause While Taking the Pill
Menopause is officially diagnosed after 12 months without a menstrual period, but if you’re on the pill, especially a combined hormonal pill, you may still have monthly withdrawal bleeding that mimics a period or you may have no periods because you decided to skip your period (learn more at #Periodsoptional).
Here’s how to tell if you might be approaching menopause:
- Perimenopause symptoms despite being on the pill. For example: You notice hot flashes, night sweats, vaginal dryness, or lower libido. You lose your waist or your LDL or triglycerides shoot up.
- Changes in your response to the pill: Your bleeding pattern shifts, becomes lighter, or disappears during your placebo week.
- Mood or sleep disturbances: Increased anxiety, insomnia, or depression—especially if they weren’t issues before.
- Age & family history: Most women reach menopause between 45 and 55. The average age is 52 years old. If you’re in your 40s and your mother reached menopause early, you might, too.
- High FSH: A follicle-stimulating hormone (FSH) level greater than 30 mIU/ml can indicate menopause, but its accuracy is reduced while on hormonal birth control. But, you can have a false negative = “normal” FSH level on birth control pills, hiding the “real” level of FSH that you would have off birth control pills, patches, rings.
If you’re unsure, you’re not alone. Many women don’t realize they’ve entered perimenopause until years later. This is where menopause-trained doctors can help with guidance, advice, and treatment.
Should I Stop Taking the Pill?
It depends on your age, health, and why you’re taking the pill.
Reasons to Consider Stopping:
- You’re over 50 and want to see if you’ve reached menopause. But please make sure you use another type of birth control until you are 1 year after your last menstrual period to prevent pregnancy, if you have heterosexual intercourse.
- You’re experiencing new symptoms that seem like menopause and you want to check your hormone level to see if you are in menopause and should switch to menopause hormone therapy (MHT).
- You’re no longer sexually active and don’t need pregnancy protection.
- You’re 50 or older and want to explore menopause-specific treatments like menopause hormone therapy (MHT). But please make sure you use birth control until you are 1 year after your last menstrual period to prevent pregnancy, if you have heterosexual intercourse.
Reasons You Might Stay On:
- You’re under 52 and still need contraception.
- The pill is helping with perimenopausal symptoms like acne, heavy and/or irregular bleeding, or cramps.
- You’ve been advised by your doctor that the benefits outweigh the risks.
Some doctors may suggest switching to a non-hormonal method (like a copper IUD) or progesterone only method or stopping the pill around age 52 to determine whether menopause has occurred. This allows natural cycles to resume so you can track periods—or the absence of them. The negative of stopping your birth control pills, patches, or rings, is that you might suffer one of the 70 symptoms of perimenopause/menopause (hot flashes, night sweats, mood changes, etc).
Birth Control Options for Perimenopausal Women
Just because you’re in your 40s or early 50s doesn’t mean you can’t get pregnant. In fact, fertility declines but doesn’t disappear until you enter menopause (doctors diagnose menopause as12 months after your last period). Birth control remains important until menopause—but your options may need to change.
Hormonal Options:
- Low-dose birth control pills: Can help regulate the irregular or heavy periods that come with perimenopause and reduce symptoms like hot flashes and night sweats in perimenopause.
- Contraceptive ring: A different delivery method (vaginal) for estrogen and progestin to stabilize the hormones during the chaos of perimenopause. There’s a monthly or yearly ring. The Nuvaring and Annovera have 20 mcg and 13 mcg of ethinyl estradiol in them vs. the “regular” birth control pills have 30-35mcg.
- Hormonal IUD (e.g., Mirena, Liletta): Provides progesterone and can prevent heavy bleeding.
- Progestin-only pills (POPs): especially for those with certain health risks who can’t take estrogen (like smokers, high blood pressure, history of blood clots).
Non-Hormonal Options:
- Copper IUD: No hormones, long-lasting but has side effects in some like more flow on your period or more cramps.
- Barrier methods (condoms, diaphragm): Less reliable but good backup during the transition or if you have infrequent sex.
- Permanent birth control: For those who are done with childbearing (e.g., vasectomy or tubal ligation).
Something to be aware of is that non-hormonal birth control options do not help with relief of menopausal symptoms. Your needs may shift as you approach menopause; it’s important to work with a doctor who understands both birth control and menopause care.
Other Menopause Treatments
Menopause isn’t just about hot flashes and periods ending—it’s a shift in hormonal balance that affects every cell in your body from the top of your head to your toes. Notably peri/menopause affects the heart, bones, brain, and mood. If you’re experiencing symptoms that aren’t controlled by the pill (or you’re off it and struggling), other treatments can help:
- Menopause Hormone Therapy (MHT): previously known as hormone replacement therapy (HRT) is a treatment that can include estrogen, with or without progesterone, to provide/supplement the hormones that your body no longer makes. It’s the gold standard for hot flashes, vaginal dryness, and bone protection/osteoporosis prevention.
- Non-hormonal medications: Certain antidepressants and anti-seizure meds reduce hot flashes.
- Lifestyle changes: Managing stress, good sleep hygiene habits, a healthy diet, and strength training can also help.
👉 Looking for expert help?
Pandia Health has doctors trained specifically in menopause care. They’ll review your symptoms, health history, and preferences to create a personalized treatment plan—from MHT to non-hormonal options. It’s all done online, discreetly, and without long wait times. Our doctors who provide asynchronous telemedicine usually take care of you within 3-5 business days vs. 3-6 month wait for an in person visit.
Takeaway
Being on the pill or other hormonal birth control can make it harder to recognize perimenopause and menopause—but it doesn’t mean you’re not going through it. If you’re in your late 40s or 50s and noticing changes, it’s worth checking in with a menopause specialist. You don’t need to guess or go through it alone.
Key reminders:
- Birth control can delay or mask menopause symptoms.
- You may need to stop the birth control pill to confirm menopause.
- There are tailored contraceptive and treatment options for perimenopause and menopause.
- You deserve care that understands your hormones, your history, and your goals.
Pandia Health is here for that exact reason—specialized, evidence-based care from doctors who get what you’re going through. Don’t wait any longer, get started today!
Disclaimer: This article is for informational purposes only and does not substitute professional medical advice. Always consult with a healthcare provider for personalized medical guidance.