Medically reviewed by Sophia Yen, MD, MPH – Written by Pandia Health Editorial Team. Updated on February 11, 2020
Research has shown an association between birth control pill use and breast cancer. However, that increased risk is very small and smaller than the increased risk of breast cancer from drinking 3 to 6 alcoholic beverages a week!
1.” Association does not equal causation” is a key tenet in science. There has not been a randomized clinical trial putting some women on the pill and some women not on the pill and assessing breast cancer risk. Only an association has been shown.
Example: those who carry lighters have an association with lung cancer. It’s not that the lighters cause cancer. It’s that people who carry lighters are usually smokers. Smoking causes lung cancer.

A confounder that could be causing this is that “women who delay having children are at greater risk of breast cancer.” Because, once you get pregnant, your breasts change and that protects you from breast cancer. So the earlier you have babies, the less your risk of breast cancer.
Per the Dana-Farber Cancer Institute, “the older a woman is when she has her first baby, or if a woman never has a pregnancy, the higher her risk for breast cancer. ” And who is best at delaying babies? Answer: those women on hormonal birth control.
2. Harvard Women’s Health Watch in 2018 had a great article on “the link between birth control and breast cancer.” TLDR: the risk is very small. Also, if you have a history of using birth control and it’s been 5 years off, then don’t worry.
Studies suggest birth control pills pose a very low risk of increasing breast cancer likelihood
In a research study in Dec 2017 of the New England Journal of Medicine studying 1.8 million Danish women, 15-49 years old, following them for an average of 10.9 years, they found an association with an increased risk for breast cancer in those that used the birth control pill, birth control patch, birth control ring, progestin-only implants, IUD with progestin, and the birth control shot.
The risk is small = increase of 13 cancers per 100,000 women who use hormonal contraception for a year or 1 extra case of breast cancer each year per 7690 women who use hormonal birth control.
This is smaller than the increased risk of breast cancer from drinking 3 to 6 alcoholic beverages per week = 22 per 100,000 person-years.
Breast cancer risk varies according to age. The risk is lower for younger women. It increases the longer you use hormonal birth control. If you use hormonal contraception for at least 5-10 years, it may take 5-10 years for your risk to go to baseline once you stop birth control.
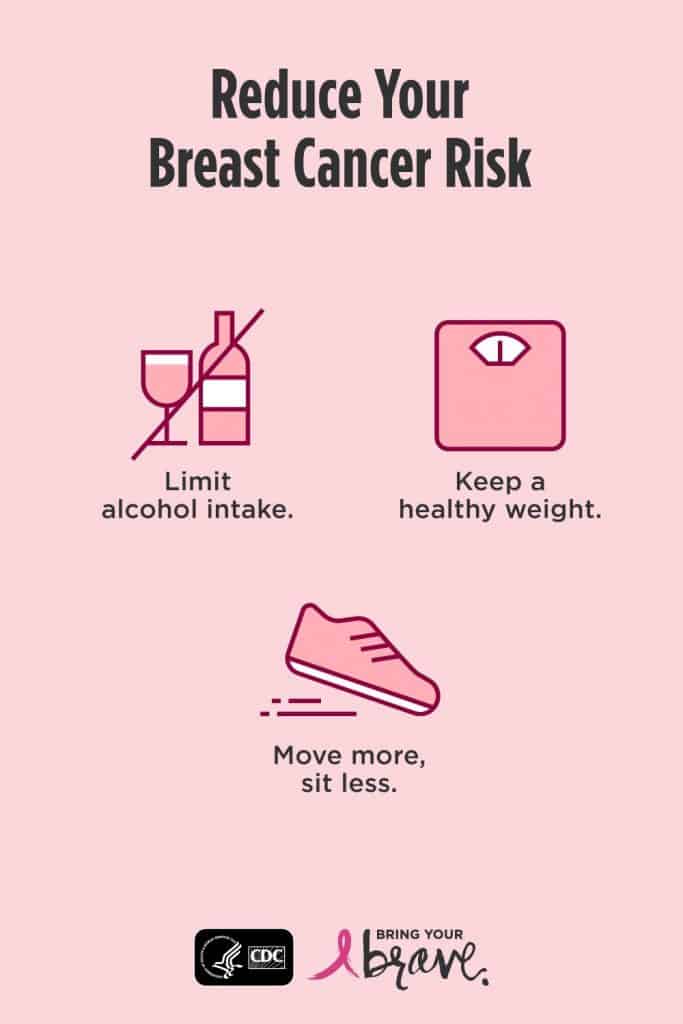
There are ways to decrease your risk of breast cancer
Don’t gain more than 5-20 pounds after the age of 18. If you do, then your risk of breast cancer increases by 40%
Adding 3-4 hours of moderate or more vigorous activity each week could reduce your breast cancer risk by 20-30%.
What if I have a family history of Breast Cancer?
If your mother, aunt, sibling has breast cancer, you are at higher risk of breast cancer.
If it is your grandmother and NOT mother, aunt, or sibling, then your risk is “average” = not higher than your person without a “family history” of breast cancer. However it could also be that your mother, aunt, siblings are still young (<62 to 70 years old) and it hasn’t shown up yet.
The cancer question is a risk/benefit analysis.
Birth Control Pills Bring About Many Benefits
With use of the birth control pill, there is decreased risk of ovarian, endometrial, and colorectal cancer.
However, one of the risks of being on the birth control pill, patch, ring and skipping the last week is increased exposure to estrogen. There has been an associated increase risk of breast cancer while on the medication, but it goes back to baseline when you are off the birth control pills for 5 years.
If there is a family history is BRCA1 or 2, in a meta-analysis study of 2855 breast cancer cases and 1503 ovarian cancer cases from 18 studies, use of Oral Contraceptive Pills (OCPs) was associated with significant reduced risk of ovarian cancer for BRCA1/2 carriers. And a 36% reduction for every 10 years used.
They found NO significant association between birth control pills and breast cancer risk in carriers. The OLDER (before 1975 formulations) had an association but NOT the newer formulations.
However, a study of 888 Jewish women with BRCA1 and BRCA2 mutations found 1.85 hazard ratio of breast cancer related to ever use of OCPs and 1.55 Hazard ration for paternal inheritance of BRCA, controlling for birth year, age at menarche, breastfeeding, and number of births.
Memorial Sloan Kettering Cancer Center’s website says: “Oral contraceptives may be taken to reduce the risk of ovarian cancer. However, it remains uncertain whether oral contraceptives have an impact on breast cancer risk in BRCA mutation carriers.”
The CDC says even if you have a family history of breast cancer, it’s is category 1 (safe) to continue or start birth control pills (CHC).
What should you do with this information?
If you are under 40 years old, just continue as you are. “The benefits of hormonal contraception in preventing unwanted pregnancies and associated complications, … lowering risk of ovarian and endometrial cancers, will outweigh this very small increased risk of breast cancer,” Dr. Nancy L Keating, a Professor of health care policy and medicine at Harvard Medical School and a physician at Brigham and Women’s Hospital, said.
If you are 40 or older or have a family history of breast cancer, you might want to consider non hormonal contraception such as: Copper IUD, condoms, surgical options (vasectomy, tubal ligation).
Starting 10 years after you STOP taking birth control pills your breast cancer risk goes back to baseline
“research found that 10 years or more after women stopped using birth control pills, their breast cancer risk returned to the same level as if they had never used birth control pills.” from webMD
If you’re interested in learning more about your birth control options and how to make your periods optional let us help you.
The above information is for general informational purposes only and is NOT a substitute for professional medical advice. Always seek the advice of your doctor/primary care provider before starting or changing treatment.

